Hard to Swallow
1
View details
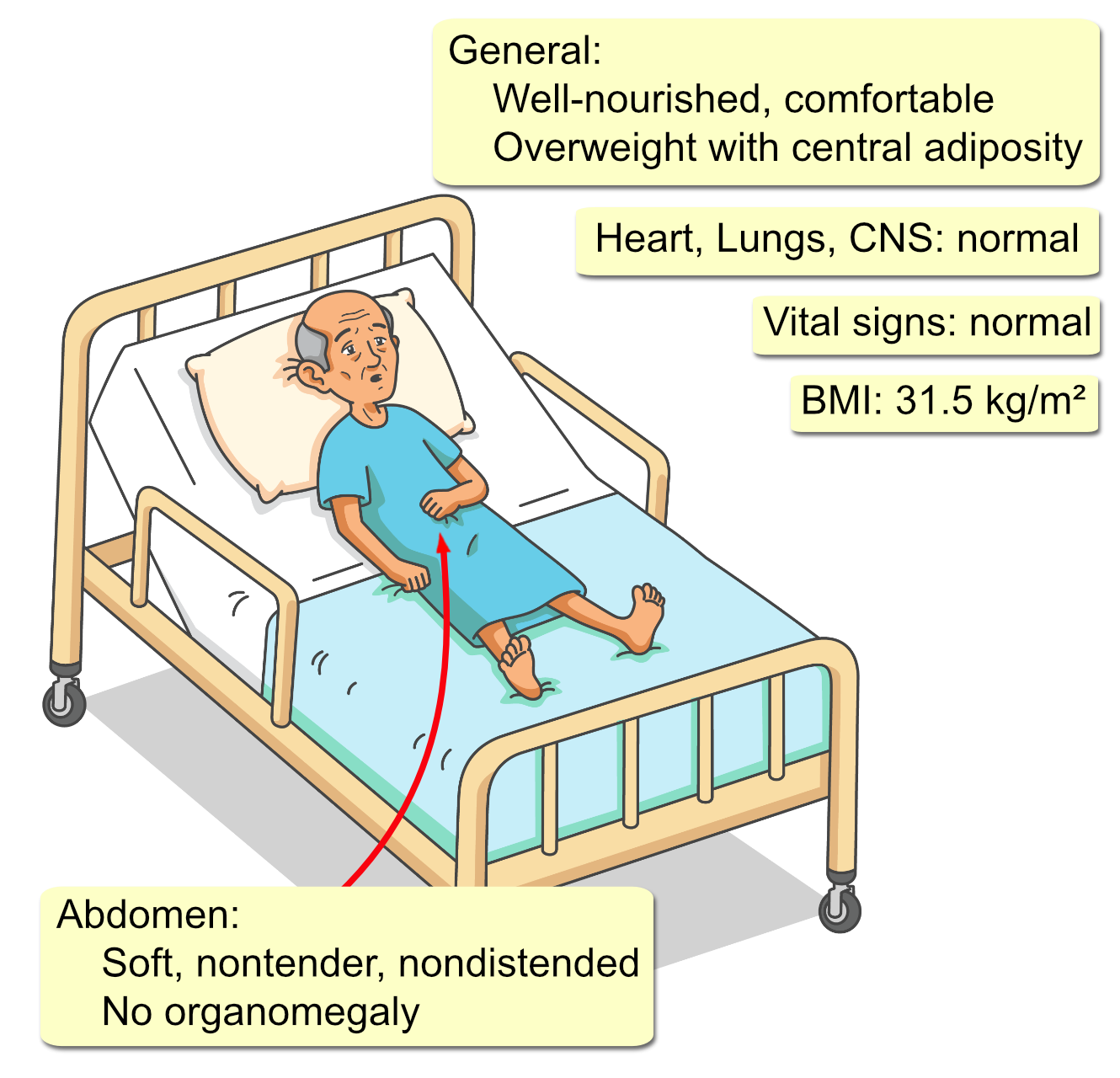
A 62-year-old Caucasian man presents to his primary care physician with a six-month history of intermittent dysphagia. He describes a sensation of solid foods, particularly bread and meat, “getting stuck” in his chest, which resolves after drinking water. He denies odynophagia. He notes an unintentional weight loss of approximately 5 pounds over the past year. He attributes this to subconsciously avoiding problematic foods. The patient has a 20-year history of gastroesophageal reflux disease, characterized by frequent heartburn. He self-manages it with over-the-counter omeprazole and has good symptom control. His past medical history is significant for hypertension and hyperlipidemia. His smoking history is 15 pack-years, though he quit 10 years ago. He drinks alcohol socially. His family history is negative for esophageal or gastric cancers.